The ROCCA test is being hailed as a groundbreaking development in ovarian cancer surveillance, offering hope to women with inherited genetic risks who face difficult decisions about their reproductive health.
Rolled out first at University College London Hospital (UCLH), the test aims to detect ovarian cancer earlier, reduce late-stage diagnoses, and provide reassurance to women carrying the BRCA1 and BRCA2 gene mutations.
For many women, ovarian cancer is known as the “silent killer” because it often presents no symptoms until it reaches an advanced stage. By then, treatment options are limited and survival rates are lower.
The introduction of the ROCCA test could significantly change this landscape, offering women more control and peace of mind.
Understanding the Risk for Women with BRCA Mutations
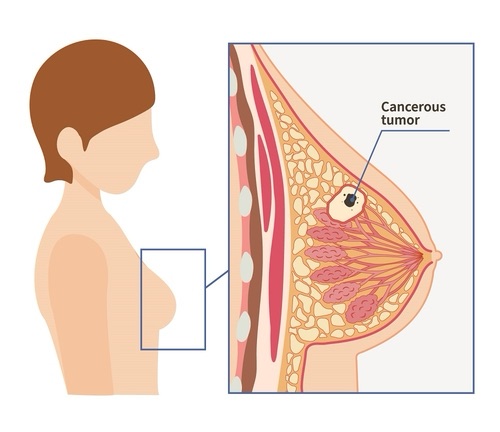
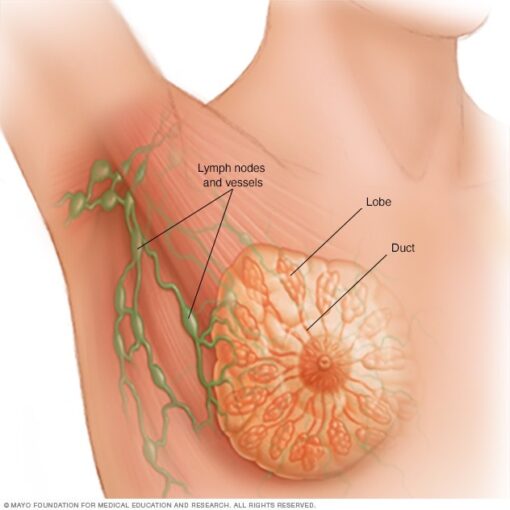
Women who carry the BRCA1 or BRCA2 mutations have a much higher chance of developing both breast and ovarian cancers compared to the general population.
Current NHS guidance often advises these women to undergo preventative surgery, involving the removal of ovaries and fallopian tubes. While this drastically reduces cancer risk, it also comes with life-altering consequences:
It triggers early menopause, with all its associated health impacts.
Women who are still planning families lose the option to have children naturally.
Many women therefore choose to delay surgery, but this leaves them exposed to the ongoing risk of ovarian cancer. This is where the ROCCA test becomes invaluable.
How the ROCCA Test Works
The ROCCA test—short for Risk of Ovarian Cancer Algorithm—is designed to provide ongoing ovarian cancer surveillance for high-risk women. Unlike the standard CA125 test, which simply measures a static level of a protein associated with ovarian cancer, ROCCA tracks how that protein changes over time.
Here’s how it works:
- Women take a blood test every four months.
- The test measures the CA125 protein marker, a substance that can indicate cancer activity.
- Results are analysed alongside a woman’s age and menopausal status.
- The algorithm then calculates an individual’s likelihood of developing ovarian cancer.
By focusing on changes in the marker, rather than a single reading, the ROCCA test provides a far more accurate assessment of cancer risk over time.
Early Evidence and Promising Results
Clinical studies have shown that women who undergo the ROCCA test have a 50% lower chance of being diagnosed with late-stage ovarian cancer compared with those relying on traditional methods. This is a crucial breakthrough because early detection vastly improves treatment outcomes and survival rates.
Equally important, the test helps women make informed decisions about when—or if—they should undergo preventative surgery.
Instead of living with uncertainty, women can now rely on regular surveillance to guide their choices.
What This Means for Women Today
At present, the ROCCA test is only being offered at UCLH in London. However, the hope is that these pilot screenings will soon expand into a national programme, making the test available to thousands of women across the country.
For women delaying surgery, the test provides a vital safety net. Every four months, it gives reassurance and clarity, bridging the gap between wanting to preserve fertility and protecting against cancer.
For healthcare professionals, it is an additional tool to personalise patient care. Doctors can track trends in a woman’s risk profile, ensuring interventions are timely and better tailored to individual circumstances.

Comparing ROCCA with the Standard CA125 Test
The traditional CA125 blood test has been used for years but comes with major limitations. Levels of CA125 can fluctuate for reasons unrelated to cancer, such as menstruation, endometriosis, or benign cysts. This has led to both false positives and missed cases.
The ROCCA test, by contrast, monitors changes over time. It’s not the absolute number that matters but the trend. This makes it a much more reliable method of ovarian cancer surveillance, particularly in women already predisposed to the disease.
The Wider Impact on Women’s Health
The introduction of the ROCCA test is about more than early cancer detection. It represents a shift in how the NHS is approaching women’s health and hereditary cancer risk. By offering this new screening option, the healthcare system is acknowledging the complex personal decisions women face when balancing cancer prevention, fertility, and quality of life.
Women with BRCA mutations often feel they must choose between reducing their cancer risk and preserving their ability to have children. The ROCCA test helps ease that burden, offering an interim measure that provides both time and security.
Looking Ahead: Will ROCCA Be Rolled Out Nationwide?
While the test is currently limited to UCLH, experts and patient groups are optimistic about a wider rollout. If introduced across the NHS, the ROCCA test could transform ovarian cancer surveillance for thousands of women in England.
Scaling up the programme would also generate more data, helping refine the algorithm and possibly extending its use beyond BRCA carriers to other women at elevated risk.
Conclusion
The ROCCA test is a landmark step in ovarian cancer surveillance. For women with BRCA mutations, it offers the chance to catch cancer earlier, avoid unnecessary surgeries, and make informed choices about their futures.
Though still in its early stages, this innovation reflects a broader move towards personalised medicine, where prevention and monitoring are tailored to each individual’s unique risk profile. With hopes of a nationwide rollout, the ROCCA test could become one of the most significant advances in women’s cancer care in years.
More news at Swiftreportnow


